Executive summary
Health spending, and the performance of the NHS, will feature prominently in the upcoming general election campaign. Many different factors matter for NHS performance and for the wider health of the population, but one important factor is the level of spending on health services. In this IFS pre-election briefing, we examine UK government health spending over the past seven decades. We then discuss the outlook for health spending over the years to come.
Key findings
1. Over this parliament, real-terms UK health spending (i.e. spending adjusted for economy-wide inflation) has grown below the long-term average rate (2.4% per year over this parliament, versus an average of 3.6% over the longer term). But the UK’s poor economic performance means that health spending as a share of national income has increased by more than the long-term average (by an average of 0.13 percentage points per year compared with an average of 0.06).
2. Over the past four decades, health spending has shown a clear tendency to rise faster than planned. But in recent years higher than expected inflation has reversed this trend. The Department of Health and Social Care (DHSC) budget has grown by less than planned over this parliament, with cash top-ups insufficient to offset the effects of higher inflation. Conservative party plans at the 2019 general election implied that the day-to-day DHSC budget (for England) would rise by 3.3% per year in real terms; latest plans imply average growth of 2.7% per year between 2019–20 and 2024–25. This is a marked departure from the experience of recent decades.
3. As well as growing in real terms and relative to the size of the economy, health spending has risen as a share of government spending over time. The DHSC’s day-to-day budget has risen dramatically from a 26% share of the all-departmental total in 1998–99 to 43% in 2022–23. Delivering health services has become a larger and larger part of what the government does.
4. Capital spending has long been much more volatile than day-to-day health spending. After being cut back sharply in the 2010s, capital spending has increased in recent years – though in 2023–24, the capital budget in England was raided to fund day-to-day pressures, returning to the bad practice of the late 2010s. One consequence of low capital spending is the deterioration of the NHS estate in England, where the maintenance backlog has more than doubled over the past decade. Within that, the ‘high-risk’ backlog has quintupled.
5. Health spending per person has been consistently higher in Scotland, Wales and Northern Ireland than in England since the start of devolution, though the gap in spending has narrowed over time. In 1999–2000, Scotland spent 22% more per person than England, Wales spent 12% more and Northern Ireland spent 15% more. But in 2019–20, on the eve of the pandemic, Scotland spent just 3% more, while Wales and Northern Ireland each spent 7% more.Within England, NHS spending this year is planned to be 32% higher per person in the area with highest funding (Cheshire and Merseyside) than in the area with lowest funding (Buckinghamshire, Oxfordshire and Berkshire West).
6. Making international comparisons of government health spending is challenging, but the available data suggest that the UK has moved up the ranks of health spending among comparable countries over the last three decades, going from comfortably below the European average in the early 1990s, to around the average in the mid-2000s, and slightly above average from the late 2000s onwards. Since the start of the pandemic, UK health spending has surged further up the (European) ranks, standing behind only France and Germany in 2022. It remains to be seen whether this will persist into future years.
7. There are no published plans for health spending in England beyond this year (2024–25) when the current Spending Review period ends. Although the Chancellor announced additional funding for new technology in future years in the Spring Budget – a sensible area to focus attention – there were no pre-existing budgets to serve as a meaningful counterfactual, which makes it difficult to assess whether this funding is genuinely ‘additional’.
8. Further increases in health spending are almost certain. The NHS workforce plan for England, which both main UK parties have endorsed, implies real-terms funding increases of around 3.6% per year if it is to be achieved. This is equal to the long-run average increase in health spending, but much larger than the increases provided since 2010, and would need to be delivered amidst weaker economic growth than we enjoyed in the past. Over the longer term, the Office for Budget Responsibility (OBR) estimate that health spending will have to rise further to meet demographic and cost pressures. Although neither major political party has provided any detail on their plans for NHS funding, whoever is in office following the general election will have to confront this in the Spending Review due by the end of the calendar year.
9. The size of the NHS means that any increases in health spending will force difficult fiscal trade-offs elsewhere. Under the government’s current plans for public service spending from next year onwards, delivering the NHS workforce plan in England implies flat real-terms budgets for all other government departments. Taking into account other spending commitments on childcare, defence and elsewhere implies large real-terms cuts to remaining departments. To avoid these cuts to other departments would require a higher overall spending envelope, which in the absence of a marked improvement in economic growth would need to be funded by some combination of increased borrowing or higher taxes.
1. Introduction
The NHS is by far the largest public service in the UK and health is consistently rated as one of the most important issues facing the country by the public (YouGov, 2024). This means that health has long been, and will continue to be, a major election issue. The Prime Minister has made improving NHS performance a key target, for example, while one of the Labour Party’s five national missions is to ‘get the NHS back on its feet’ (Prime Minister’s Office, 2023; Labour Party, 2024).
The health of the UK population is driven by many factors, one of which is the quantity and quality of healthcare that the NHS can provide. One obvious factor that determines this is the amount of funding made available to the system. Making use of that funding productively and efficiently is also extremely important, and the government is right to focus on that with the current public sector productivity review. But the level of funding inevitably matters too.
Health spending has significance beyond its impact on health services. Given the sheer size of the NHS relative to the rest of the public sector, decisions over NHS funding have outsized fiscal implications: for the availability of funding for other public services, and for levels of tax and government borrowing. The NHS is an increasingly large part of what the government does, and this means that health spending decisions inevitably force hard trade-offs elsewhere, particularly amidst such a challenging fiscal outlook (Emmerson et al., 2024).
In this report, we focus on government spending on health services in the UK. We first set out seven key facts about health spending. These cover how health spending has changed over time, how it varies across different parts of the UK and how the UK compares with similar countries. We then outline the outlook for health spending in England, including current plans, the implications of the NHS workforce plan and longer-run pressures on health funding.
Where possible, we use measures of UK-wide health spending. In places, data limitations and/or a lack of UK-wide spending plans mean that we focus on England alone. This choice is further motivated by the fact that health is a devolved matter, and so plans for England are most relevant for an election for the Westminster parliament. Some spending measures have been adjusted for changes in definitions or methodology over time and so may not match those in official documents or, indeed, past IFS publications.
2. Seven facts about health spending
1. UK government health spending has risen rapidly – but unevenly – over the past 75 years
Health spending has grown rapidly over the past 75 years, increasing in real (inflation-adjusted) terms fourteen-fold between 1949–50 and 2022–23. The proportion of national income devoted to public health spending has also more than doubled over that period. Recent years have seen real-terms health spending grow at below the long-term average rate (2.4% per year over this parliament, versus an average of 3.6% over the longer term) but have also seen health spending grow faster relative to the rate of economic growth than during most periods of the past.
UK government spending on health has increased considerably over time. In real terms (i.e. after adjusting for economy-wide inflation), spending has increased almost fourteen-fold over the past 70 years, rising from £16.5 billion in 1949–50 (in today’s prices) to £225.0 billion in 2022–23. Health spending has also grown faster than the economy as a whole, and so has grown to account for a greater share of national income: public spending on health grew from 3.6% of national income in 1949–50 to 7.3% in 2019–20, on the eve of the pandemic, and to 8.2% in 2022–23. In the other words, the share of national resources devoted to health has more than doubled over the lifetime of the NHS. This is illustrated in Figure 1.
By health spending, we are here referring to the definition used for the internationally agreed ‘classifications of the functions of government’.1 This is a relatively broad definition that includes spending on what we might call ‘core NHS services’ (e.g. hospitals and GP surgeries) as well as public health services, community health services and medical equipment. During the pandemic, it included spending on the vaccine programme, personal protective equipment (PPE) and the ‘Test and Trace’ programme, which contributed to the pronounced spike in real-terms spending in 2020–21 and 2021–22. Spending has fallen back since as those pandemic-era programmes have been unwound.
Even putting the pandemic to one side, health spending has not grown at an even pace over the years. The rate of growth has fluctuated over time. This is summarised in Figure 2, which shows (in the top panel) the average growth in real-terms health spending by parliament and (in the bottom panel) the average rate of growth of health spending as a share of national income by parliament. The former tells us how quickly the resources provided to the health service grew in each period. The latter tells us the extent to which health spending grew faster than the wider economy, which tells us something about the extent to which health spending was prioritised (as it is easier to provide larger funding increases when the economy and tax revenues are also growing rapidly).
UK health spending has grown at an average real-terms rate of 3.6% per year since 1949–50 (top panel of Figure 2). Spending has grown at a slower rate than that during every parliament since 2010, and grew by an average of just 1.0% per year during the 2010–2015 Coalition government. Over this current parliament – defined as 2019–20 to 2024–25 – the most recent set of spending plans implies an average real-terms growth rate of 2.4% per year. This compares to an average 7.9% between 2001–02 and 2005–06, the parliament with the fastest average growth rate.
We see a somewhat different picture if we instead look at growth in health spending as a share of national income (bottom panel). On this measure, recent years have seen above average increases in health spending: although real-terms health spending hasn’t grown all that quickly relative to the rates of growth seen in the past, it has grown rather more quickly relative to the size of the economy. Historically, health spending has increased as a share of national income by an average 0.06 percentage points each year. Over this parliament, funding is set to grow by an average of 0.13 percentage points of national income per year. This reflects the UK’s poor economic performance of late, and the fact that health funding has continued to grow despite that (not least because of the pandemic, plus the pressures of an ageing population). The increases have still been far below those seen during the final two terms of the last Labour government, however.
2. Health spending grew faster than demographic pressures over the 2000s and early 2020s – but not during the 2010s
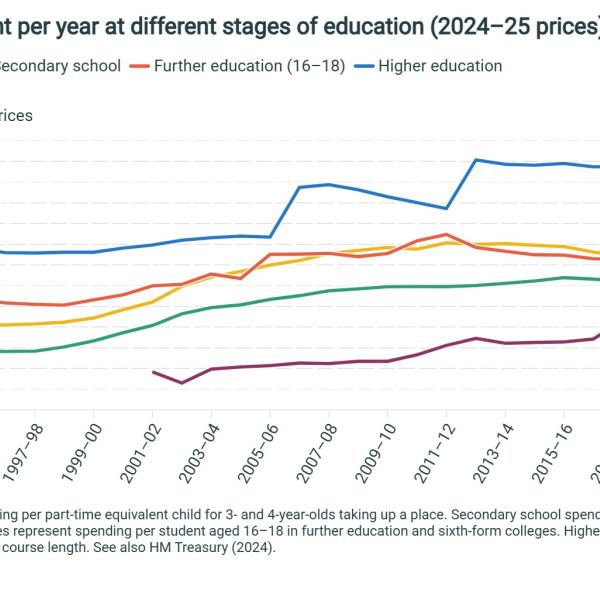
Bigger and older populations have greater healthcare needs. The UK’s growing and ageing population is a key driver of growing demands upon the health service. Over the 2000s, funding grew faster than demographic pressures. Between 2010 and 2019, growth in health spending was only just enough to keep pace with a growing and ageing population. Since then, funding growth has outpaced demographic pressures, but this does not account for other increases in demand arising from the pandemic or wider trends in population health.
Examining changes in the level of real-terms health funding does not provide a complete picture: we also need to consider the changing demands being placed upon the budget. One key source of changes in demand is demographics. Most obviously, a larger population will demand more healthcare. But for a given population size, an older population will tend to demand more healthcare (as older people are less likely to be in good health, more likely to have medical conditions that warrant care, and more likely to have needs that complicate the delivery of that care).
One way to account for this is to construct a measure of age-adjusted spending per person – a measure of spending that accounts for the changing age composition of the population as well as its size. To do this, we attach a weight to each population group based on how much healthcare they use on average (using estimates of health spending by age published by the OBR). This provides an estimate of the amount by which funding would need to increase in order to keep pace with demographic pressures. For instance, over the period between 2001–02 and 2022–23, health funding would have needed to grow by 0.6% per year in real terms just to keep pace with the overall size of the population, and by 0.9% per year to keep pace with both population growth and the ageing of the population.
It is important to note that this does not capture everything: it will not capture changes in population health conditional on age (e.g. worsening or improving levels of illness at a given age, or changes in healthy life expectancy),and it will not capture changes in health-specific cost pressures (e.g. from the discovery of new drugs or medical technologies). These other pressures will also affect how health spending compares with demand and so this analysis is only partial. But this analysis still gives us a better sense of the extent to which funding is keeping pace with demand than looking at real-terms health funding alone.
Figure 3 shows how real-terms UK health spending has evolved relative to these demographic pressures. The green line shows how real-terms spending evolved, the yellow line shows the evolution of real-terms spending per person and the blue line shows the evolution of age-adjusted real-terms spending per person.
Over the 2000s, funding grew at a considerably faster rate than demographic pressures: age-adjusted spending per person increased substantially. Over the 2010s, the rate of funding growth slowed and growth in demographic pressures accelerated. As a result, age-adjusted spending per person (the blue line) was broadly flat between 2009–10 and 2018–19, before ticking upwards in 2019–20 (to be around 5% higher than in 2009–10). Since then, age-adjusted spending has increased sharply, though interpretation of this is complicated by the pandemic (which has created a whole raft of pressures on the service beyond those associated with demographics).
3. Health spending per person varies substantially across the UK
Health spending per person has been consistently higher in Scotland, Wales and Northern Ireland than in England since the start of devolution in 1999, though the gap in spending has narrowed over time. Within each of the four parts of the UK, health spending also varies between different areas. In England, NHS spending this year is planned to be 32% higher per person in the area with highest funding (Cheshire and Merseyside) than in the area with lowest funding (Buckinghamshire, Oxfordshire and Berkshire West). This variation across local areas reflects differences in assessed need for healthcare services, as well as differences in the costs of providing services.
So far, we have focused on health spending in the UK as a whole. But the amount spent on health services per person varies substantially across different part of the UK. In part this is because areas have different needs for healthcare funding, either because of differences in the health needs of their populations or differences in the costs of providing healthcare. But also, different areas – particularly the devolved nations – make different political decisions, most obviously about how much to spend on healthcare relative to other services, and also how much to raise in taxes.
The funding and provision of health services has been devolved to Scotland, Wales and Northern Ireland since 1999. Over the past 25 years, these devolved governments have made decisions about the funding and organisation of health services that differ from the decisions the Westminster government has made for health services in England. Figure 4 shows health spending per person in England, Scotland, Wales and Northern Ireland since 1999–2000.
Panel (a) shows real health spending per person, while panel (b) shows real spending per person relative to England.
Consistent with the UK-wide trend discussed in the previous facts, health spending per person has generally grown over time in each of the four nations of the UK. But in each nation, it grew much faster between 1999–2000 and 2009–10 than between 2009–10 and 2019–20. During the COVID-19 pandemic, health spending in all four nations increased substantially, and although it fell back in 2022–23, in all cases it remained much higher than pre-pandemic.
Scotland, Wales and Northern Ireland all spent more per person on health than England throughout this period (£38, £293 and £184 more in 2022–23, respectively). But this gap in spending between the devolved nations and England has shrunk over time. At the dawn of devolution in 1999–2000, Scotland spent 22% more per person than England, Wales spent 12% more and Northern Ireland spent 15% more. But in 2019–20, on the eve of the pandemic, Scotland spent just 3% more, while Wales and Northern Ireland each spent 7% more. This is because health spending per person has grown faster in England (from a lower base) than in the devolved nations.
One reason for differences in health spending across the four nations may be that the populations of the different nations have different needs for healthcare services. Figure 5 therefore adjusts health spending per person for the age distribution of each nation, in the same way we did in Figure 3. This accounts for differences in the age structure of the population, but not for differences in the needs of people at each age, or for differences in the costs of providing services.
For Scotland and Northern Ireland, health spending per person remains higher than England throughout this period even after adjusting for differences in age. For Northern Ireland, age-adjusted health spending is more generous relative to England than non-age-adjusted health spending, as was the case for Scotland up to 2007–08. This means that the age structure was more favourable – in terms of requiring less health spending – than in England. Or, put more simply, Northern Ireland spends more per person despite having a younger population.
For Wales throughout this period, and Scotland from 2008–09, age-adjusted health spending is less generous relative to England than non-age-adjusted health spending. This means that the age structure was less favourable than in England. Indeed, for Wales between 2012–13 and 2015–16, health spending per person was less generous than England after this age-adjustment despite headline per-person spending being higher than in England. So, in other words, in these years it appears that higher per capita spending in Wales could be more than fully explained by their population being older than that in England.
Within each nation, health funding and resources also have to be allocated to local areas. Details differ between each of the four nations but, in each case, funding is allocated based on the estimated need for healthcare services and the costs of providing them. This depends on political decisions about how different factors should be weighted.
Here, we focus on the allocation of funding with England, but similar approaches are taken in Scotland, Wales and Northern Ireland. Within England, most NHS funding is allocated each year by NHS England to 42 Integrated Care Boards (ICBs) that each organise and fund health services for people living in their geographical area. This allocation of funding to ICBs is based on a complex assessment of the need that each area has for different types of health services, as well as differences in the cost of providing services. Additional funding is then provided with the explicit objective of reducing health inequalities.2
Figure 6 shows the allocation that each area is planned to receive per person in 2024–25. This covers most, but not all, NHS services. There is a large variation in funding per person. At the extremes, the ICB for Buckinghamshire, Oxfordshire and Berkshire West is planned to receive £1,597 per person, while the ICB for Cheshire and Merseyside is planned to receive £2,102 per person, 32% more. The NHS funding allocation system is relatively well designed and most – but not all – of these differences in funding are based on differences in assessed need. These differences in assessed need are in turn driven, by, amongst other things, differences in the age and deprivation of populations in each area.
Public health funding is allocated to local authorities separately to the allocation of NHS funding and goes towards a range of preventative services such as children’s health programmes, obesity and activity programmes and alcohol and drug misuse services. Total public health funding (£3.6 billion in 2024–25) is much smaller than NHS funding (£164.9 billion in 2024–25). The allocation methodology for public health funding is much worse than that for NHS funding: it is now more than a decade out of date, and many local authorities receive far more or far less funding than they would under up-to-date assessments of their need. For more details on the funding allocation methodologies and resulting distributions of funding for both the NHS and public health, see Ogden et al. (2022, 2023).
4. Capital spending has been more volatile than day-to-day spending
Capital spending on health amounts for around 5% of the total. The level of capital spending has grown in recent years, after being cut back in the early 2010s. In the late 2010s, spending was increasing, but funding was repeatedly transferred out of capital budgets to meet day-to-day spending pressures – a practice that was repeated in 2023–24. The consequences can be seen in the deterioration of the physical NHS estate, where the maintenance backlog has more than doubled over the past decade.
The vast majority of UK health spending – between 94% and 96%, depending on the year – is classified as ‘resource’, or day-to-day, spending (Figure 7). This includes the ongoing costs of providing healthcare – the most significant being staff wages, which make up almost half (45%) of the entire NHS England budget (Department of Health and Social Care, 2023). The remainder of UK health spending (between 4% and 6% of the total) is classified as ‘capital’ spending. This can be thought of as investment in fixed assets – things such as hospital buildings and medical equipment.
Whereas day-to-day spending on health has tended to rise steadily over time (albeit at a fluctuating rate), capital spending is more volatile. This can be seen in Figure 7: after more than trebling over the 2000s (a 262% increase in real terms between 1999–00 and 2009–10), capital spending on health was cut by 30% between 2009–10 and 2016–17. Capital spending has increased since and was 68% higher in 2022–23 than in 2016–17, and 18% higher than in 2009–10.
The feast-and-famine nature of capital funding could conceivably make it more difficult to plan and to deliver investments in the NHS estate effectively. A further concern is that the health service in England has (with the agreement of HM Treasury) displayed a repeated tendency to dip into capital budgets to help meet pressures on day-to-day budgets, something that is not supposed to be possible under the government’s spending control framework. These capital-to-resource transfers amounted to £0.6 billion in 2014−15, £1.2 billion in 2015−16 and 2016−17, £1 billion in 2017−18 and £0.5 billion in 2018−19.
Speaking to the Public Accounts Committee in September 2023, Shona Dunn, Second Permanent Secretary at the DHSC, told MPs that capital-to-resource transfers were ‘not something that we would want to do as part of normal financial management’, ‘certainly not something that we now do’ and ‘not something that we would want to return to’(Public Accounts Committee, 2023). Despite these protestations, in the 2023–24 Supplementary Estimates published in February 2024, it was revealed that almost £1 billion had been transferred from the capital to the resource budget to meet in-year spending pressures – a return to the practice of the past. For more detail on these in-year spending pressures, including those related to the costs of industrial action in the sector, see Gainsbury (2023).
Capital expenditure in the UK health system is below the average for advanced economies (Warner and Zaranko, 2021). There are signs that the level of capital spending has been insufficient to maintain the quality of the physical NHS estate: the estimated amount of investment required to eradicate the NHS England maintenance backlog has more than doubled from £5.4 billion in 2013–14 to £12.5 billion in 2022–23 (both in 2024–25 prices). This increase, shown in Figure 8, also includes a quintupling of the high-risk backlog since 2010. Rather concerningly, this is defined as cases ‘where repairs/replacement must be addressed with urgent priority in order to prevent catastrophic failure, major disruption to clinical services or deficiencies in safety liable to cause serious injury and/or prosecution’.
One particular area of concern with regard to the NHS estate is the presence of reinforced autoclaved aerated concrete (RAAC) and the associated safety risks. Following widely reported issues in school buildings built between the mid-1950s and mid-1990s, many NHS hospitals have searched for and discovered RAAC in their buildings. According to the latest data, there are 54 hospital sites in England with confirmed RAAC, with 31 of these sites identified since mid-2023 (Department of Health and Social Care, 2024). DHSC have announced £700 million of funding until 2025 to mitigate and remove RAAC from NHS buildings in England (Tidman, 2024), but the overall impact on the maintenance backlog remains to be seen.
This deterioration in the quality of the NHS estate and the inadequate levels of capital investment more generally are likely to be part of the explanation for the NHS’ disappointing productivity performance in recent years (Warner and Zaranko, 2022, 2023; Patel, 2024).
5. Health spending typically grows faster than planned – though not in recent years
Health spending has not only tended to rise over time, but it has also tended to grow at a faster rate than originally planned. Over the four decades prior to the pandemic, health spending in England on average grew by 1.4 percentage points more per year, in real terms, than originally planned. In recent years, though, this pattern has reversed. Because the health budget is set in advance in nominal (cash) terms, much higher than initially expected inflation in recent years has meant that health spending has grown by less in real terms than planned, and top-ups have been insufficient to offset this.
Historically, health spending has displayed a clear tendency to grow by more than originally planned. This was true right from the creation of the NHS: the 1950 Conservative party manifesto noted that ‘Every year the Estimates laid before Parliament [for the NHS] have been greatly exceeded’ (Conservative Party, 1950). It has also been true of the last few decades. This is illustrated in Figure 9, which compares plans and out-turns for real-terms growth in health spending since the early 1980s. Since 1999, this covers health spending in England only.
Over the four decades or so prior to the pandemic, on only two occasions (the 1991 Autumn Statement and the 2004 Spending Review) did health spending grow more slowly than planned. Instead, the NHS budget was typically topped up and spending grew by more than originally planned. Over the pre-pandemic period, health spending on average grew by 1.3 percentage points more than planned a year previously.
Data for the pandemic period itself need to be interpreted with caution. Spending Review 2019 set plans in England for the 2020–21 financial year. These plans were, for obvious good reasons, not adhered to. In the event, huge additional sums were allocated to fund the pandemic response. Non-COVID-19 health spending (which is what is shown in Figure 9) actually fell in England in 2020–21, as COVID-19 patients took precedence over routine procedures and appointments and millions of patients stayed away. Spending Review 2020 set plans for 2021–22. In the event, health spending grew more slowly than planned in real terms, largely because inflation (as measured by the GDP deflator) was higher than expected (or, more accurately, not quite as negative).
The period since 2021–22 is more instructive and more striking. The 2021 Spending Review set plans for 2022–23, 2023–24 and 2024–25. Real-terms resource funding for the DHSC (covering health services in England) was planned to grow by 4.1% per year in real terms. The latest plans now suggest that funding will instead grow by 2.7% per year over the three years. This is not because the NHS has had its cash budget reduced. It is because inflation has turned out so much higher than expected. The health service has received some additional cash funding as a result (Warner and Zaranko, 2022), but not enough to return real-terms growth to the rate set out in the 2021 Spending Review. It is possible that the health service will receive a substantial in-year top up for 2024–25, but it would take a top-up of more than £7 billion to return average real growth over the period to 4.1% (as originally planned). This seems unlikely. Instead, it is more likely that this Spending Review period will see health spending grow less quickly than initially planned, something that has only happened a handful of times outside of the pandemic.
Another way to think about the recent evolution of health spending is to compare with what was promised at the 2019 general election. IFS analysis at the time noted that Conservative party plans implied average real-terms growth in the total DHSC budget (TDEL) of 3.1% per year between 2019–20 and 2023–24 (Farquharson, 2019). Within that, those plans implied growth in the day-to-day budget (RDEL) of 3.3% per year. On the assumption that these plans would have been extended for another year, this implies pre-election plans were for real-terms funding growth of 3.3% per year between 2019–20 and 2024–25. The government’s latest plans imply average growth in the DHSC resource budget of 2.7% per year over that period (and average growth in the total DHSC budget of 3.0% per year).
In other words, despite a pandemic, record waiting lists and growing rates of ill health, real-terms day-to-day health spending in England has risen no quicker than was planned five years ago. To reiterate, this is not because the health service has seen its cash budget pared back. Cash spending in 2024–25 will, in fact, be more than £8 billion higher than implied by Conservative plans at the last election. The point is that this additional funding has been insufficient to offset unexpectedly high rates of inflation.
6. Health spending accounts for an ever-greater share of spending on public services
Health spending has not only risen over time in both real terms and as a share of national income, but it has also risen as a share of government spending. For example, health spending has risen from 8% of total spending in 1955–56 to 18% in 2022–23, and from 13% to 29% of (a broad definition of) public service spending. In other words, delivering health services has become a larger and larger part of what the government does.
In our first fact, we showed that health spending has risen substantially over time, both in real terms and as a share of national income. It is also the case that health spending has risen as a share of total government spending over time. In other words, delivering health services has become a bigger and bigger part of what the government does over time.
Figure 10 shows three measures of health spending as a share of total government spending. The yellow line shows UK health spending as a share of total managed expenditure (TME), the total amount of money that the government spends each year. This covers spending on public services, social security, interest on government debt and investment. The green line shows UK government health spending as a share of public service spending alone (defined here as TME minus spending on social security, debt interest and investment). The blue line then shows the DHSC’s day-to-day spending budget (which covers health spending in England) relative to day-to-day spending by all government departments.
For each measure, the rise in health spending as a share of government spending is clear. UK health spending has risen from 7.8% of TME in 1955–56 to 18.1% in 2022–23, having peaked at 32.1% in 2021–22. Over the same period, UK health spending rose from 12.6% of public service spending to 29.3%. The DHSC’s day-to-day funding has risen from 26.3% of departmental day-to-day spending in 1998–99 to 42.8% in 2022–23. Under current plans, this will remain approximately constant, at 42.9% in 2024–25.
7. Making international comparisons of health spending is challenging, but available data suggest the UK has moved up the ranks of health spending over time
It is difficult to interpret international differences in health spending, not least because no single measure is perfectly comparable across different countries and systems. Differences in spending may be driven by differences in healthcare needs, differences in the efficiency of healthcare systems or genuine differences in the quality of healthcare provision, but can also reflect differences in how data are collected and constructed (across both countries and time). With those caveats in mind, the available data suggest that in the early 1990s, UK public health spending as a share of national income was below the EU14 average and one of the lowest in the G7. Since then, the UK has moved up the ranks, and between the late 1990s and the COVID-19 pandemic, the UK government spent a larger share of national income on health than the EU14 average. During the pandemic, the UK has risen even further up the ranks, although it remains to be seen whether this will persist in future years.
In this fact, we examine how UK health spending compares with other countries. International comparisons are difficult, not least because the way that health systems are organised and funded differs substantially across countries. What counts as ‘public’ health spending is not always clear-cut. To remain broadly consistent with our previous analysis, we focus on health spending that is either publicly funded through taxation (such as the vast majority of the NHS) or funded through compulsory insurance schemes. This excludes out-of-pocket or voluntary private health spending.
International comparisons are also challenging because of differences in data collection. In line with most analyses of health spending and resources across countries, we use health data collected by the OECD. These are the best available data but should still be interpreted with caution, given the frequent changes in the methodology and data used for different countries over time.
One reason that countries differ in how much they spend on healthcare is their different national incomes. It is much easier to spend more on healthcare (in pounds and pence) when you have a greater national income (and thus greater ability to raise taxes), and much harder when you have a lower national income. Many countries that the UK is often compared with – including Germany, the Netherlands, Canada, Australia and all Nordic countries – had higher GDP per person in 2022 (World Bank, 2024). All else being equal, we might therefore expect these countries to spend more on healthcare services in per person terms than the UK. For this reason, we focus on public/compulsory health spending as a share of GDP, which allows us to look at the extent to which public health spending is prioritised given the available resources of each country.
Figure 11 shows public/compulsory health spending as a share of GDP in selected countries between 1990 and 2022. Panel (a) shows G7 countries excluding the United States (as there was a major reclassification of health spending in the US in 2014 following reforms to health insurance). Panel (b) shows EU14 countries and their median.
Starting first with panel (a), the UK has tended to spend a lower share of GDP on health than most other G7 countries. For periods of the 1990s, the UK spent the lowest share of GDP on healthcare (vying with Japan and Italy for the bottom spot). In the 2000s, the UK moved up the international rankings and overtook Canada, Italy and Japan, before being overtaken by Japan in the 2010s. On the eve of the COVID-19 pandemic, in 2019, the UK still spent substantially more than Italy and slightly more than Canada. During the pandemic, health spending in the UK shot up, overtaking Japan. But by 2022, health spending had fallen back and the UK returned to the same position among G7 countries as it had pre-pandemic. Throughout this whole period, from 1990 to 2022, Germany and France consistently spent a larger share of GDP on public/compulsory health.
Turning to panel (b), the shaded area shows the range of health spending among EU14 nations, while the yellow line shows the median spending. The UK spent a relatively low share of GDP on public/compulsory healthcare among the EU14 until 1997, when it moved to around the EU14 average. Between 1997 and 2004, the UK broadly tracked the EU14 median, before overtaking it consistently. Although health spending as a share of GDP flattened and even fell in the 2010s, this happened in many European countries, and the UK remained above the EU14 median. During the pandemic, the UK rose rapidly up the health spending ranks, and in 2022 spent the third highest share of GDP on public/compulsory health, behind only France and Germany. It remains to be seen whether this was a temporary effect of the pandemic (perhaps because of how pandemic spending was recorded in different countries), or whether the UK will now consistently spend much more on health than the EU14 average. As well as reflecting the genuinely large increase in UK health spending during the pandemic, this rise up the international ranks was likely also driven by the UK’s relatively slow GDP growth since the start of the pandemic (House of Commons Library, 2024).
Taken together, the results suggest that the UK spends a consistently smaller share of GDP on public/compulsory healthcare than France and Germany. Prior to the start of the COVID-19 pandemic, UK public/compulsory health spending was close to Canada, and higher than Italy and the EU14 average. Data since the start of the pandemic suggest that the UK has spent more than nearly all EU14 countries on public/compulsory healthcare in recent years, though it remains to be seen how that will change in the coming years that are less affected by COVID-19.
We have focused on public/compulsory healthcare spending in this section. But different countries rely on private healthcare spending to different extents, and this can change over time. Ultimately, for population health, it is the total level of healthcare spending that matters most. In 2022, total UK healthcare spending amounted to 11.3% of GDP, of which 2.1% was private (i.e. classified as voluntary or out-of-pocket); the equivalent figures for 2019 were 10.0% (total) and 2.1% (private).
If we look at international trends, the patterns remain very similar to those discussed above. Since the 1990s, the UK increased its total health spending as a share of GDP and moved up international ranks, rising from near the bottom of the EU14 to just below the median from the mid-2000s. Since the start of the pandemic, UK total health spending has also moved rapidly up the ranks, and in 2022 total UK health spending as a share of GDP was below just France, Germany and Austria among EU-14 nations.
3. The outlook for health spending
We now turn to the outlook for health spending in both the short and long term. Because this report aims to provide context for the upcoming UK-wide general election, we focus on the outlook for health spending in England, for which Westminster is responsible. Elections for devolved parliaments are more relevant for health spending plans in Scotland, Wales and Northern Ireland.
What has been announced?
Budgets for government departments are set in a spending review, which tend to occur every couple of years. These plans may then be topped-up down the line. The current spending review period runs until 2024–25, and the next spending review is not planned until after the general election. As a result, there are no published plans for health spending in England for 2025–26 and beyond. Figure 12 shows the day-to-day budgets for the DHSC and NHS England. Under current plans, these will remain approximately constant in real terms between 2023–24 and 2024–25, though are still substantially above their pre-pandemic levels.
The government has, however, set out its plans for overall public spending from 2025–26 to 2028–29. These are needed for the OBR to produce forecasts for the aggregate public finances and to assess the government’s performance against its target to have public sector net debt excluding the Bank of England falling in the fifth and final year of the forecast period. This overall funding envelope is relatively tight, allowing total day-to-day departmental spending to grow by 1.0% per year in real terms. As we discuss later, this means that the next government will face challenging trade-offs when deciding on how much to increase health spending.
One exception to this lack of plans for 2025–26 onwards came in the March Budget this year. The Chancellor set out that the NHS in England would receive £3.4 billion of ‘additional funding’ for technological and digital transformation. This focus on improving NHS productivity through capital and digital investment is sensible. There was a corresponding top-up to the government’s overall plans for capital spending, so in that sense it is ‘additional’, though without any baseline for the NHS to compare against, it is impossible to know whether this is meaningfully ‘additional’ for the health service or whether it would have happened anyway.
The NHS long-term workforce plan and longer-term trends
Although there are currently no formal budgets for health spending beyond this year, the first NHS long-term workforce plan, published in June 2023, sets out the government’s plans for the future of the NHS in England. The plan sets out the NHS’ own assessment of how the NHS workforce will need to grow between 2021–22 and 2036–37 to meet the growing demand for services and to address existing workforce challenges. Although the plan included additional funding for expanding training places, it did not estimate the funding implications of such a large increase in the workforce.
In previous work, we have estimated the funding implications of the plan (Warner and Zaranko, 2023). In our central scenario, we estimated that the NHS workforce plan implies a real-terms funding increase for NHS England of 3.6% per year between 2021–22 and 2036–37. This is equal to the long-run average annual real-terms increase in UK health spending discussed in our first fact about health spending. It would imply that by 2036–37, NHS spending in England increases by around 2 percentage points of GDP.
The workforce plan therefore implies that health spending will grow in line with the long-run average, and as a result would require growth in spending that is considerably higher than the rates seen since 2010. There is, however, uncertainty around these estimates. How much funding will be needed to deliver the plan depends both on how much NHS wages will need to rise and on how much non-staffing spending (e.g. spending on equipment) will also need to increase. We therefore produced alternatives to our central scenario. In our ‘low scenario’, we estimated that funding would have to increase by an average of 2.4% per year in real terms, closer to the growth rate achieved in recent years. But in our ‘high scenario’, we estimated that NHS funding would have to increase on average by 4.4% per year, a level of growth not seen since the new Labour governments between 1997 and 2010.
Both the government and the Labour party have endorsed the workforce plan. Our costings of the plan suggest that this means the NHS budget would have to grow significantly in real terms on average each year in the coming decade, if the plan is to be delivered. But the range of uncertainty is large, and ultimately depends on whether other aspects of the plan – such as ambitious training, retention and productivity targets – are achieved.
In the longer term, it is almost certain that NHS funding will need to continue to rise in real terms if the NHS is to deliver the same level of services as it currently does in the face of an ageing, sicker population and rising costs of delivering health services. Figure 13 shows the OBR’s projections for future UK health spending as a share of GDP, produced in 2023 on the basis that current policy (i.e. current levels of provision) is maintained. The OBR project that by 2071–72 the government will spend 14.8% of GDP on providing healthcare, compared with 8.2% in 2023–24. This corresponds to an average real growth rate of around 3.0% per year, slightly below our estimate of the funding increases needed to deliver the NHS workforce plan.
What does this mean for the spending review?
The next government will need to hold a spending review soon after taking office, to set departmental budgets and agree a local government finance settlement for the fiscal year beginning in April 2025 (and possibly later years, though a one-year settlement seems likely given the accelerated timeframe). This will include deciding budgets for the DHSC and NHS England.
By definition, for a given overall spending plan, any increases in health spending must reduce spending on all other departments. The size of the NHS relative to other areas of spending
(Fact 6) makes this trade-off particularly large.
Figure 14 illustrates this trade-off graphically. The government has pencilled in a 1% real-terms annual growth in day-to-day departmental spending from 2025–26 (the light green line). If the DHSC receives a real-terms annual growth rate of 3.1% (enough to give NHS England 3.6%, as per our estimates of the cost of the workforce plan, as long as other health budgets are frozen in real terms), this would imply zero real-terms growth for all other departments – in other words, flat real budgets. This is the yellow point on the chart. After considering other spending commitments – on childcare, defence and international aid – this would imply substantial real-terms cuts for other departments.
To increase spending on other departments, there are two options. The government could either increase NHS spending by less (for example, the red point), or increase the total funding envelope by more (the blue point). In the absence of an improvement in the economic outlook, topping up the funding envelope would require some combination of higher borrowing or higher taxes. Trade-offs between additional health spending and spending on other government departments therefore present a difficult choice for the next government. Readers can explore these trade-offs for themselves using the new IFS ‘Be the Chancellor’ tool.3
4. Conclusion
We should perhaps not place too much weight on the parties’ stated pre-election plans. Things can and do change – not least when something like the COVID-19 pandemic comes along. At the 2019 general election, Conservative party plans implied a 29% increase in the cash size of the day-to-day DHSC budget between 2019–20 and 2024–25. Given inflation expectations at the time (a cumulative 10% over the five years), that would have delivered average real-terms increases of 3.3% per year. The government’s latest plans imply a 37% increase in the cash budget, but much higher-than-expected inflation (20% over five years) has wiped this out, leaving average real growth of 2.7% per year. That’s comfortably below the 3.9% average real growth promised by Labour at the last election, and below the 3.6% long-run average.
This time around, neither the Conservatives nor Labour have (at the time of writing) provided such detail about their plans. The current NHS budget only runs until this year. Beyond that, no official plans exist, and no unofficial plans have been forthcoming. But the historic trend is clear: health spending rises over time, and more often than not, faster than the size of the economy, and faster than planned. In the face of demographic and other cost pressures, spending will need to rise just for the service to stand still. And even standing still would leave the NHS performing considerably worse than it was pre-pandemic, despite some recent progress in cutting the overall waiting list (Warner and Zaranko, 2024). The NHS workforce plan – which both the Conservative and Labour parties have committed to – is, in effect, a recognition of this, and implies substantial real-terms funding increases over time. Such increases though will inevitably force hard fiscal decisions to be made elsewhere – decisions that all political parties are keen to postpone until after the general election.
The overall funding envelope is important. But as we have discussed, how funding is spent – including the geographical allocation and the split between capital and resource – matters a lot too. Higher funding does not automatically translate into more activity or better outcomes, as the recent challenges with NHS productivity have demonstrated (Warner and Zaranko, 2023). The government’s focus on improving productivity is therefore welcome. But any plausible increase in productivity does not change the fact that – absent a large change in the role of the NHS, or further deterioration in quality – health spending will need to continue to rise over time.