The national Accident and Emergency (A&E) four-hour waiting time target is once again in the news headlines. Performance against this recently fell to the lowest since records began, with only 79.8% of patients in December 2019 admitted, discharged or transferred to another hospital within 4 hours as opposed to the 95% standard.
Recent comments from the Health Secretary Matt Hancock suggest that the existing target is likely to be scrapped, echoing the interim recommendations of an ongoing review into NHS clinical targets that would replace the target with new goals that focus on reducing initial treatment times for severe cases and introducing an average waiting time target for all patients.
But what does the target – and any potential changes to it – actually mean for patients? While this target is often used as a benchmark for overall hospital performance, a working paper by researchers at the IFS, Cornell University and the Massachusetts Institute for Technology (MIT) suggests that the target has meaningful impacts on patient outcomes. This paper studies the impact of the target on the treatments received by patients and their subsequent survival outcomes, and finds that the target was successful in reducing A&E waiting times, but increased the number of inpatient admission and costs. These impacts were accompanied by a large reduction in the mortality rate of A&E patients. These mortality reductions appear to be driven by shorter waiting times rather than additional treatment, and mostly affect patients with severe and potentially time-sensitive conditions such as sepsis and stroke. This suggests that the current target is playing an important role in reducing waits and improving mortality outcomes for high severity patients. As set out here, it is important that policymakers understand the relative costs and benefits of the current arrangement when considering potential changes to the target to ensure that any new incentives placed on hospitals help to deliver the best possible outcomes for NHS patients.
Since 2010, all major NHS A&E departments are meant to discharge, admit or transfer at least 95% of patients within four hours of arrival. The solid line in Figure 1 shows the distribution of A&E waiting times in 2011-12 and 2012-13 – a period of time in which most hospitals were meeting the target - for all patients in major NHS hospitals. The target creates an obvious spike in waiting times just prior to four hours, with more than 10% of patients being admitted, discharged or transferred to another hospital in the final 10 minutes before reaching the target. This is in sharp contrast to the estimates of the distribution if the policy was removed (as shown by the smooth, dotted line). As a result, we estimate that the target reduced average waiting times by approximately 20 minutes over this period of time. The target has therefore been successful in achieving its primary aim of reducing waiting times.
Figure 1: The observed and estimated counterfactual distribution of A&E waiting times
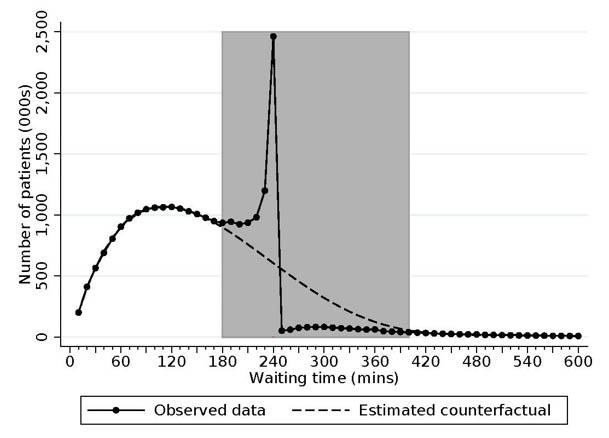
Source: Figure 1 of J. Gruber, T. P. Hoe and G. Stoye (2018)
However, the target also has further impacts. These are summarised in Figure 2. This shows that the target increased the number of inpatient admissions by around 12%, with a corresponding fall in discharges and transfers to other hospitals. While these additional admissions were often for minor patients who did not receive much expensive treatment during their hospital stays – and who were plausibly only admitted so that they wouldn’t breach the target – these extra visits still increased the average patient cost by £95, a 5% increase on an average cost of around £1,900 for each patient affected by the target.
Strikingly, the target also led to large reductions in the number of patient deaths. Patient mortality within a year of visiting A&E fell by 0.3 percentage points among the patients affected by the target, reducing the probability of mortality among this group from 9% to 8.7% as a result of the policy. Given the large number of A&E patients affected by the target each year, these estimates imply that the target resulted in around 15,000 fewer deaths in 2012-13 alone. The cost of achieving this was broadly in line with the cost of a life-year estimates routinely used in deciding which NHS treatment to fund (between £20,000 and £30,000 per Quality Adjusted Life Year (QALY) gained).
Figure 2: Estimated impacts of the target on inpatient admissions, costs, and patient mortality
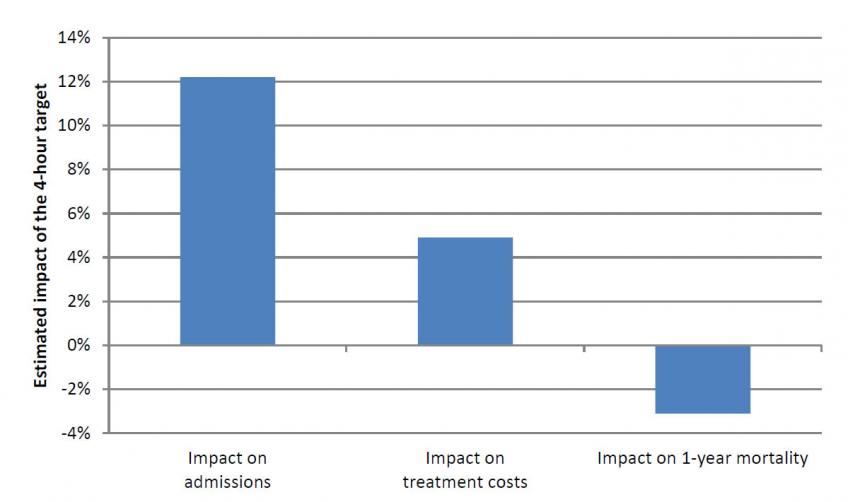
Source: Tables 3 and 4 of J. Gruber, T. P Hoe and G. Stoye (2018).
How do patients benefit from the target?
This raises the question of what is saving these lives – lower waiting times or extra admissions? To shed light on this question, the paper examines how the impacts of the target vary between patients with different diagnoses, and across different periods of time when hospitals have different levels of available space in their inpatient departments (and therefore variable ability to meet the target by simply admitting A&E patients when they approach the target). This evidence suggests that it is the bigger reductions in wait times that are associated with larger mortality reductions, while there is no relationship between admissions and deaths.
The type of patients who benefit from the policy also suggest that waiting times are key. If reduced waiting times can explain why mortality falls, we should expect to find the largest impacts of the policy among conditions which are time sensitive (e.g. strokes), and no impacts among conditions which are not (e.g. cancer). Examining the impacts of the policy across diagnoses, the paper finds that the biggest reductions in mortality rates are found among potentially serious conditions that could benefit from timely treatment, with the largest impacts found among sepsis, vascular and cerebrovascular (stroke) patients. By contrast, there is no impact on patients with a number of different cancers, serious conditions which are less time-sensitive in an acute setting. This again suggests that the four-hour target has played an important role in reducing waiting times and improving patient outcomes among patients with time-sensitive and serious conditions.
What does this mean for proposed changes to the target?
All of this suggests that the four-hour target has played an important role in improving A&E care. Waiting times have fallen, and while costs have increased, this has been accompanied by large reductions in mortality among high-severity patients. On this basis, the current target appears to be working well for patients – at least when hospitals are broadly meeting the standard.
Of course, this doesn’t mean that care couldn’t be further improved – particularly in light of recent performance against this target – or that an alternative incentive scheme couldn’t produce similar or better outcomes. However, careful thought should be given to the design of any alternative targets introduced.
While not officially confirmed, an interim report for an NHS England review into clinical targets suggests that there will be four areas targeted by the new target: (i) time to initial clinical assessment, (ii) time to emergency treatment for severe patients, (iii) mean waiting time target calculated across all patients, and (iv) utilisation of ‘Same Day Emergency Care’ to avoid overnight admissions.
Our analysis suggests that the benefits of the current target – in terms of mortality – accrue mostly to time-sensitive patients, many of which are explicitly included in the list of priority patients targeted by component (ii). Focusing attention on these patients – including conditions such as sepsis, heart attack and stroke - could therefore achieve similar, or perhaps even greater, reductions in mortality than realised under the current policy. However, thinking about how to implement this policy in practice raises questions. There is often confusion over the exact diagnosis of patients upon arrival, and identifying which patients are covered by the target might not always be obvious (and could even lead to hospitals ‘manipulating’ recorded diagnoses to better hit the target). Indeed, the current policy appears to be so effective because it means that patients who should be treated quickly – but who are not diagnosed or treated as quickly as they would optimally be – are treated faster. Mandating faster treatment times for patients with specific conditions but not others risks losing the benefit that the current policy provides for hard-to-diagnose patients.
It is also important to note that low-severity patients are rarely the ones who breach the target. In fact, a high proportion of these patients comfortably meet the current target. And while these patients may not experience mortality reductions, they often still experience some wait time improvements as a result of the policy. This benefit should not be ignored, and concerns for these patients are the justification for imposing a limit on the average (mean) time spent waiting across all A&E visits. However, there is little evidence for what the ‘right’ target time hospitals should look to achieve in order to maximise patient outcomes, or what sort of average wait time the public would find acceptable. This will no doubt be the subject of much debate as further details of any policy changes emerge.