This week the Care Quality Commission (CQC) published comparable information on all GP surgeries in England for the first time, with the aim of identifying which practices should be prioritised for newly introduced inspections. Understanding whether and why some GP practices fail to provide quality care is important given the vital role that GPs play within the NHS. In recent years, there have been substantial changes to the organisation of GP practices, with a shift away from single-handed practices towards practices with six or more full time equivalent GPs. This observation summarises the findings of an IFS report published today, which describes these trends in detail and examines the relationship between practice size and a variety of practice outcomes and behaviours.
Trends in the organisation of GP practices
Between 2004 and 2010, the total number of full-time equivalent (FTE) GPs in England grew by 15%, rising from 32,263 to 37,173 FTE GPs. Over the same period, the registered population grew by just 5%. As a result, the number of FTE GPs per individual increased by 10%.
Meanwhile, the number of GP practices fell. In 2004, 9,016 practices were registered. By 2010, this had decreased to 8,832. These trends together reflect in a shift towards a smaller number of GP practices which on average employ a larger number of GPs. In 2004, there were 3.6 FTE GPs per practice. This rose to 4.2 in 2010. In particular, there has been a marked decrease in the number of single-handed GPs, while practices with six or more FTE GPs have become more common.
In the figure below, we divide practices into four categories:
- single-handed (one or fewer FTE GPs per practice)
- small-medium (more than one and up to three FTE GPs)
- medium-large (more than three and up to six FTE GPs)
- large (more than six FTE GPs)
The share of small-medium practices and medium-large practices stayed flat between 2004 and 2010, while the percentage of single-handed GPs fell (from 22% to 15%) and the share of large practices grew (from 16% to 23%).
Figure: Share of GP practices, by FTE GPs (all practices)
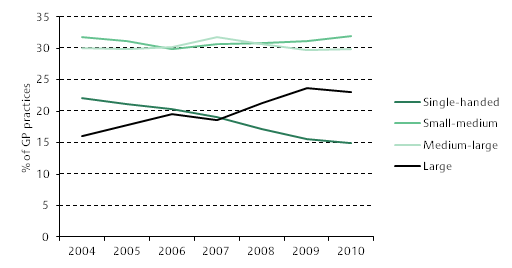
Note: Includes all GP practices with at least one registered GP in the year in question.
Source: Kelly and Stoye (2014), Figure 2.2
Practice size, behaviour and patient outcomes
Overall there is a small, positive relationship between the size of GP practices and the score that they achieve under the Quality and Outcomes Framework (QOF). QOF scores (introduced in 2004), partially determine payments to practices and are used to provide an overall measure of the clinical quality of a GP practice. We find that single-handed practices achieved the lowest average scores, while large practices achieved the highest. These findings remain even after controlling for differences in the characteristics of the populations and areas that small and large practices serve. However, there is variation across the different domains captured by QOF. Interestingly, single-handed practices achieved the highest average scores for patient experience but lower scores in the other domains. This means that patients appear to be more satisfied with the care received in small practices, despite objective measures suggesting that they receive worse clinical standards of care.
We also find some evidence that single-handed GPs are more likely than GPs in larger practices to have high emergency admission rates among their patients for conditions that would potentially have been avoidable. There are a number of conditions (known as ambulatory care sensitive or ACS, conditions) for which emergency hospital admissions are potentially preventable if the patient receives timely and effective primary care. These include acute conditions (such as ear, nose and throat and urinary tract infections), chronic conditions (such as diabetes and asthma) and vaccine preventable conditions (such as influenza). Smaller practices are found to be significantly more likely to be among the 20 per cent of practices with the highest emergency admissions rates for ACS conditions, and this relationship holds even when taking account of other patient and practice characteristics. This relationship is particularly strong in the case of chronic conditions, with single-handed GP practices 4% more likely to appear in this category relative to large practices. This perhaps suggests that practices with fewer GPs are less able to spend significant periods of time managing long-term conditions.
We also find that smaller practices behave differently from larger ones in how they refer patients on for secondary care. Single-handed and small-medium practices are, other things being equal, less likely to refer their patients for secondary care than GPs in larger practices are. For example, single-handed practices are 12% more likely to appear in the 20 per cent of practices with the lowest referral rates (once adjusting for the demographic composition of their patients).These practices are also less likely to refer patients to independent sector providers. This may indicate a lower willingness or ability of GPs in smaller practices to offer a full range of treatment options to patients.
It is important to note however that there is significant variation across practices of the same size, and some smaller practices provide extremely good quality care. There are also many factors that could affect the outcomes examined in our report, and which may differ between small and large practices. As a result, the relationships between GP practice size and GP behaviour are not necessarily causal. For example, if small practices typically treat patients with worse health on average, the findings related to higher than expected emergency admissions in small practices could simply reflect underlying health differences rather than any impacts of practice size. Other GP characteristics may also vary across different practice sizes in some unobservable way.
These findings overall suggest that smaller practice sizes typically deliver worse health outcomes for patients, particularly in single-handed practices. Although we cannot say for sure that the small number of GPs is the sole cause of this relationship, it is likely to be an important factor. It is important for policymakers to be aware of this, and understand it better so as to address it.